Gabapentin for Epilepsy: Real Talk on Benefits, Side Effects, and Dosing
By: A health writer with patient-centered insight
When it comes to treating epilepsy, there’s no one-size-fits-all answer. But if you or a loved one has been prescribed gabapentin, you’re probably wondering: What does this drug actually do? Will it stop the seizures? And what’s the deal with dosages like gabapentin 400 mg or 600 mg?
This article walks you through the essentials—from how gabapentin works to the real-world pros and cons—so you can make informed decisions with your neurologist.
1. What Is Gabapentin and Why Is It Used for Epilepsy?
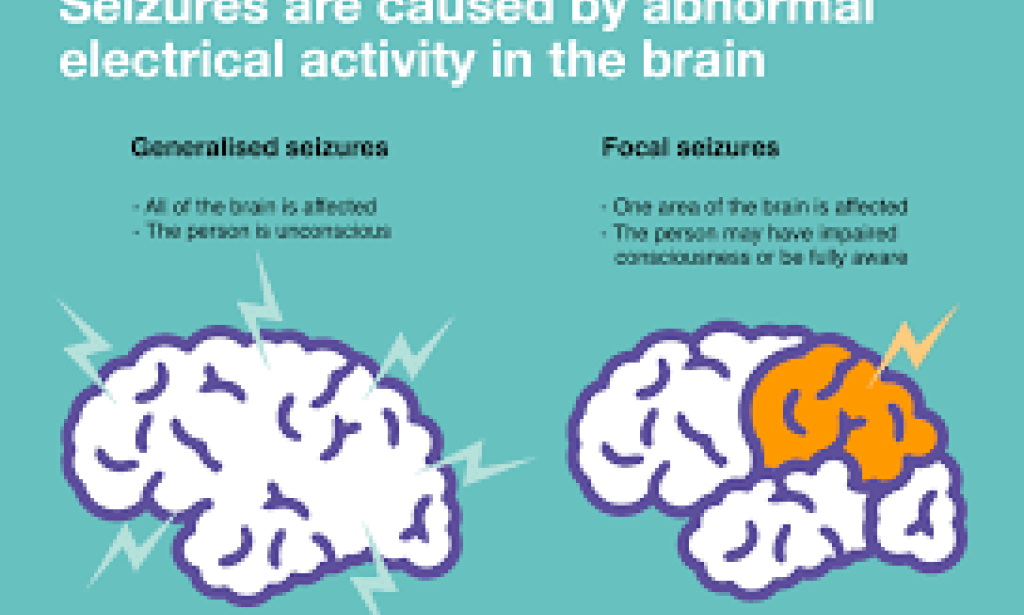
Gabapentin (you may know it by the brand name Neurontin) is an anticonvulsant medication. It’s commonly prescribed as an add-on therapy for focal seizures, especially when other medications don’t fully control the condition.
In simple terms:
Gabapentin helps calm overexcited nerves in the brain, which are often the source of seizures. It doesn’t directly mimic GABA (a calming neurotransmitter), but it binds to specific calcium channels, reducing electrical activity without making you overly sedated, especially at lower doses.
2. Gabapentin 400 mg vs. Gabapentin 600 mg: What’s the Difference?
Gabapentin dosages vary widely depending on the individual, the type of seizures, and how well the body tolerates it.
Gabapentin 400 mg
Often prescribed as a moderate daily dose, usually taken in three divided doses. For many people, 400 mg is a sweet spot—it provides relief from focal seizures without causing overwhelming side effects.
Common reasons to stay at 400 mg:
-
You’re just starting and want to ease in.
-
You have mild epilepsy or infrequent seizures.
-
You’re older or have kidney concerns (since gabapentin is processed by the kidneys).
What to expect:
✅ Fewer side effects like drowsiness
✅ Mild seizure control (when used with other AEDs)
✅ Easier on the body over the long term
Gabapentin 600 mg
This dose is typically for patients needing stronger seizure control or who didn’t see improvement at lower doses. It may be taken 2–3 times a day.
Why go up to 600 mg?
-
You’re still having seizures on 400 mg.
-
Your doctor believes a slightly higher dose might provide more consistent brain stability.
What to watch for:
⚠️ Higher risk of brain fog or memory trouble
⚠️ Some people report dizziness or coordination issues
⚠️ Side effects may creep in gradually over time
3. Brand Names Matter: Neurontin vs. Gralise vs. Horizant
Let’s clear up a common confusion: Only Neurontin (and its generics) are approved for treating epilepsy.
-
Neurontin = immediate-release = ideal for seizures
-
Gralise & Horizant = extended-release forms = used for nerve pain or restless leg syndrome (RLS), not epilepsy
Bottom line:
🟢 Use Neurontin or generic gabapentin for epilepsy
🔴 Skip Gralise or Horizant unless treating nerve pain under separate guidance
4. How Effective Is Gabapentin, Really?
Gabapentin isn’t a miracle drug, but it’s helpful for many.
🔹 It reduces seizure frequency by 30–40% for a lot of patients
🔹 About 15% of people become seizure-free when using it as part of a broader treatment plan
🔹 It works best for focal (partial) seizures, not so much for generalized or absence seizures
That said, every person reacts differently. Some do very well at gabapentin 400 mg, while others find real control at gabapentin 600 mg or higher (up to 1800 mg daily in rare cases).
5. Side Effects: What You Should Know
Most side effects show up in the first few weeks and often fade. But some can persist or sneak in later at higher doses.
Common:
-
Drowsiness or fatigue
-
Dizziness
-
Swelling in the legs or hands (edema)
-
Brain fog or slower thinking (more common at 600 mg+)
Serious (but rare):
-
Mood swings or suicidal thoughts (always report these!)
-
Allergic reactions (rash, facial swelling)
-
Breathing issues may occur if taken with opioids or other sedatives
Pro tip: Keep a daily journal for side effects and seizure activity. This helps your neurologist fine-tune your treatment safely.
6. Who Should Be Cautious with Gabapentin?
Gabapentin might not be the best fit if you:
❌ Have serious kidney problems (dosage must be carefully adjusted)
❌ Are pregnant or trying to conceive (limited safety data)
❌ Have a history of depression or suicidal thoughts
Always consult your neurologist about your full health history. There may be better alternatives depending on your specific needs.
7. Tapering: Don’t Stop Cold Turkey
Whether you’re on gabapentin 400 mg or gabapentin 600 mg, stopping suddenly is a bad idea. It can trigger seizures or cause withdrawal symptoms like anxiety, insomnia, or flu-like symptoms.
Work with your doctor to create a slow tapering plan, especially if you've been on gabapentin for several months or more.
8. Gabapentin vs. Other Epilepsy Medications
| Medication | Pros | Cons |
|---|---|---|
| Gabapentin | Fewer interactions, safer for the liver | Not great as a solo drug |
| Keppra (levetiracetam) | Broad coverage, fast-acting | Mood swings, irritability |
| Lamictal (lamotrigine) | Mild on cognition, weight neutral | Risk of serious skin rash |
| Carbamazepine | Strong for focal seizures | Liver toxicity, drug interactions |
Gabapentin shines when used as part of a combo approach, especially for patients who can’t tolerate heavier-hitting meds.
9. Practical Tips If You’re Taking Gabapentin
DO: ✔ Take it at the same time each day
✔ Drink plenty of water to reduce swelling
✔ Log how you feel physically and mentally
AVOID: ✖ Alcohol—it amplifies dizziness
✖ Skipping doses
✖ Antacids too close to your gabapentin dose—they reduce absorption
Final Thoughts: Is Gabapentin Right for You?
Gabapentin, whether at 400 mg or 600 mg, can be a gentle but effective partner in epilepsy care, especially for focal seizures. It doesn’t work for everyone, and it’s not without trade-offs. But for the right patient, it can bring stability, peace of mind, and fewer ER visits.
Remember:
There’s no shame in trying gabapentin—or in deciding to stop if it’s not the right fit. Your health journey is yours. The most important thing is working closely with your neurologist, tracking how you feel, and being honest about what’s working and what’s not.
You must be logged in to post a comment.