Hypertension is an important public health problem due to its high prevalence and its remarkable contribution to increased cardiovascular morbidity and mortality. Five class of antihypertensive drug such as diuretics, beta-blockers, calcium antagonists, ACE inhibitors, and angiotensin receptor antagonists were recommended as first-line therapies. Pharmacological action sites of these drugs lie at four anatomic control sites including heart, kidney and blood vessels. Despite, the availability of many medications for the treatment of hypertension, only 25-30% of hypertensive patients are benefitting from prescribed medications they are currently taking. That is partly due to inter-individual variation in drug response, including both efficacy and toxicity. Genetics and other factors may be important factors that determine inter-individual variation to drugs response. To overcome these issues, several investigators have tried to identify individual patient’s characteristics that predict blood pressure response prior to drug administration; however, no profile method currently recommended as a basis for selection of antihypertensive drug therapy. In addition, Clinicians must often rely on trial and error approach to identify the right drug and dose for each patient; however, side effects of drugs and wastage of time and energy are problematic in that approach.
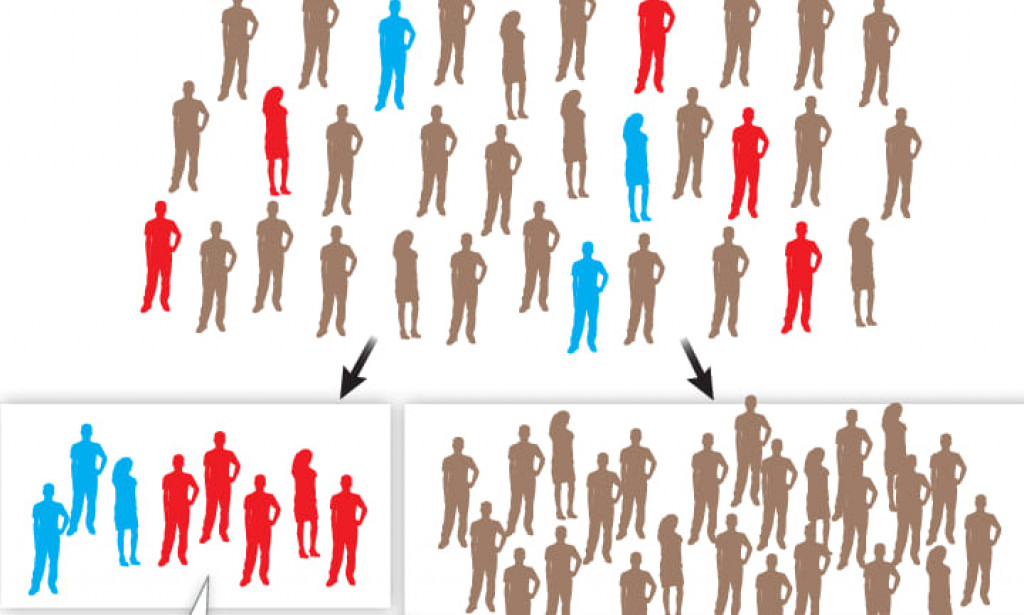
The promise of pharmacogenetics study of antihypertensive drugs lies in its potential to identify individual genetic profile that predicts the right drug and dosage to individual patient thereby maximizing clinical benefit with minimized side effects. In this review, the pharmacology (mechanism & action site) of main antihypertensive drugs and the current status of pharmacogenetics of antihypertensive drugs, mainly focusing on: ACE genes, angiotensinogen genes, angiotensen type 1 receptor genes, beta-adrenergic receptor genes and alpha-adducin gene were summarized. Although, several studies reported significant associations of ACE (I/D), AGN (M235T), AT1 (A1166C), ADRB1 (Arg389Gly Ser49Gly) & ADD1 (Gly460Trp) with different antihypertensive drugs response; however, pharmacogenetics data emerging from these studies have been mostly inconsistent. We claim that these inconsistencies results are due to poor study design, inadequate sample sizes, lack of replication, and heterogeneity amongst patient populations and phenotypes. Besides, the reviewers recommended that progress in the future will depend upon our ability to launch large studies using high-fidelity phenotyping with multiple drugs and multiple ethnic groups.

You must be logged in to post a comment.